High Implementation Costs
A primary barrier to implementing new service lines.
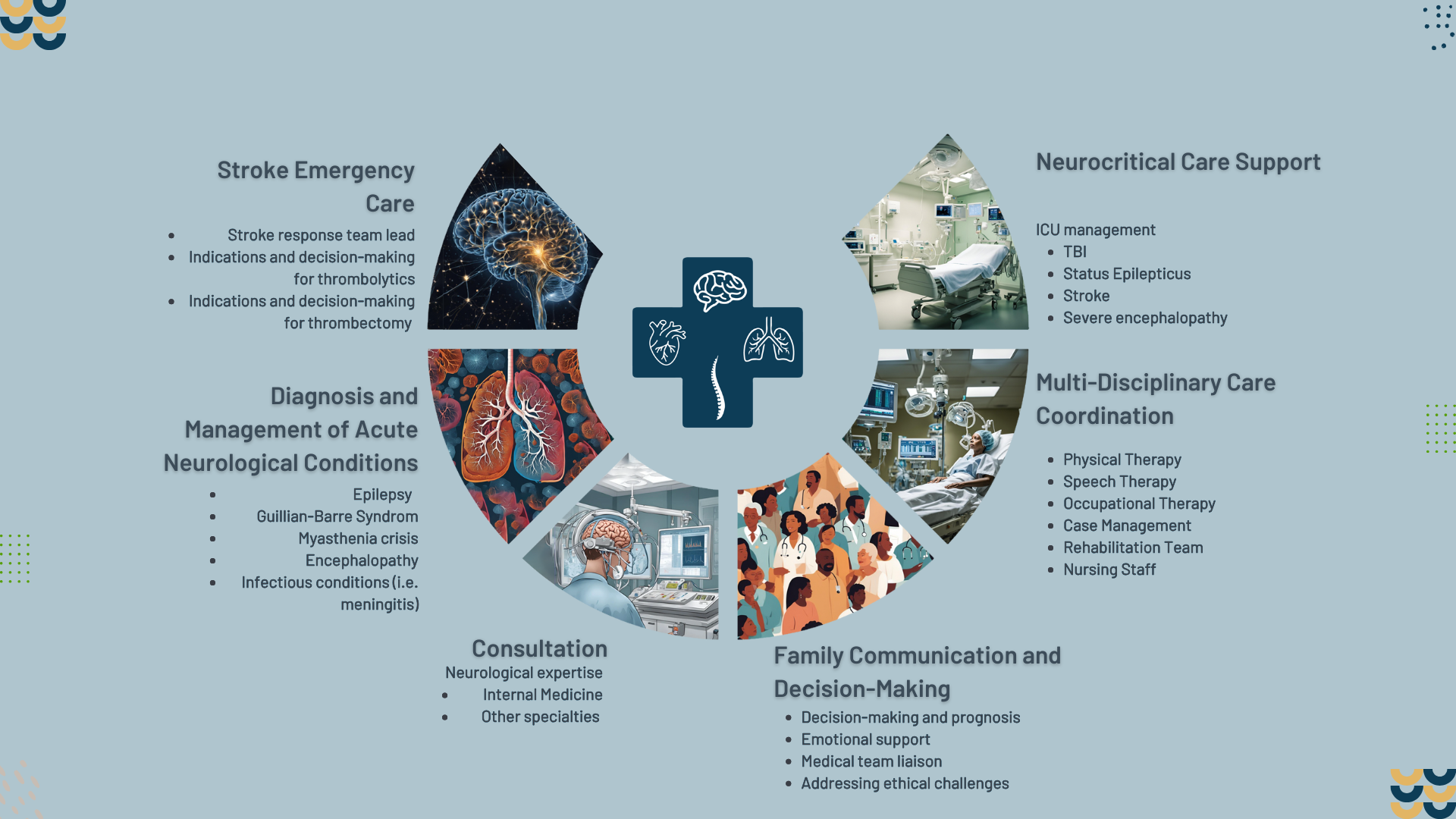
Providing 24/7/365 world class acute and critical care services to acutely ill patients, regardless of the location or capabilities of the acute care setting.
We envision a future in which all hospitals providing acute and intensive care have 24/7/365 access to experts in any medical specialty via telemedicine.
Hospitals face a variety of challenges related to skyrocketing costs, lower reimbursement, provider shortages, and technology needs. The NEUCARES platform provides creative solutions to many of these problems.
Service line expansion is costly, requiring assembly of a specialized team, construction of high-cost facilities, and provision of dedicated administrative support. Transferring patients to specialized centers can introduce additional risks and complexities. Collaboration with external professional providers can be difficult due to technological issues, slow response times, and administrative challenges.
A primary barrier to implementing new service lines.
Burn out. Shortages in essential tools, treatments, and specialists.
May lead to increased costs and loss of revenue.
Technological issues, slow response times, and administrative hurdles.
The growing numbers of chronically ill, aging, and disparaged members of the U.S. population pose a threat to the ability of hospitals to provide needed acute and critical care services.
Rising hospitalization rates among patients with progressive conditions such as CHF and COPD
Health care providers face a growing strain related to rising rates of disease burden and acuity, aging populations, less providers entering the field to replace retirees, provider burnout and exit from the profession, and crushing administrative demands on time and energy. They also face job dissatisfaction related to pay and quality of life.
Higher ICU utilization-5
10% increase in the last 10 years
Older, sicker patients
Projected physician shortages of up to 124,000 by 2034
Administrative burden
Physician shortages
Heavy schedules
Lack of autonomy
Moral distress
Decreasing pay
Inequality between pay and workload
Poor quality of life
NEUCARES provides a world-class customized platform for acute and critical care services 24/7/365 via telemedicine nationwide.
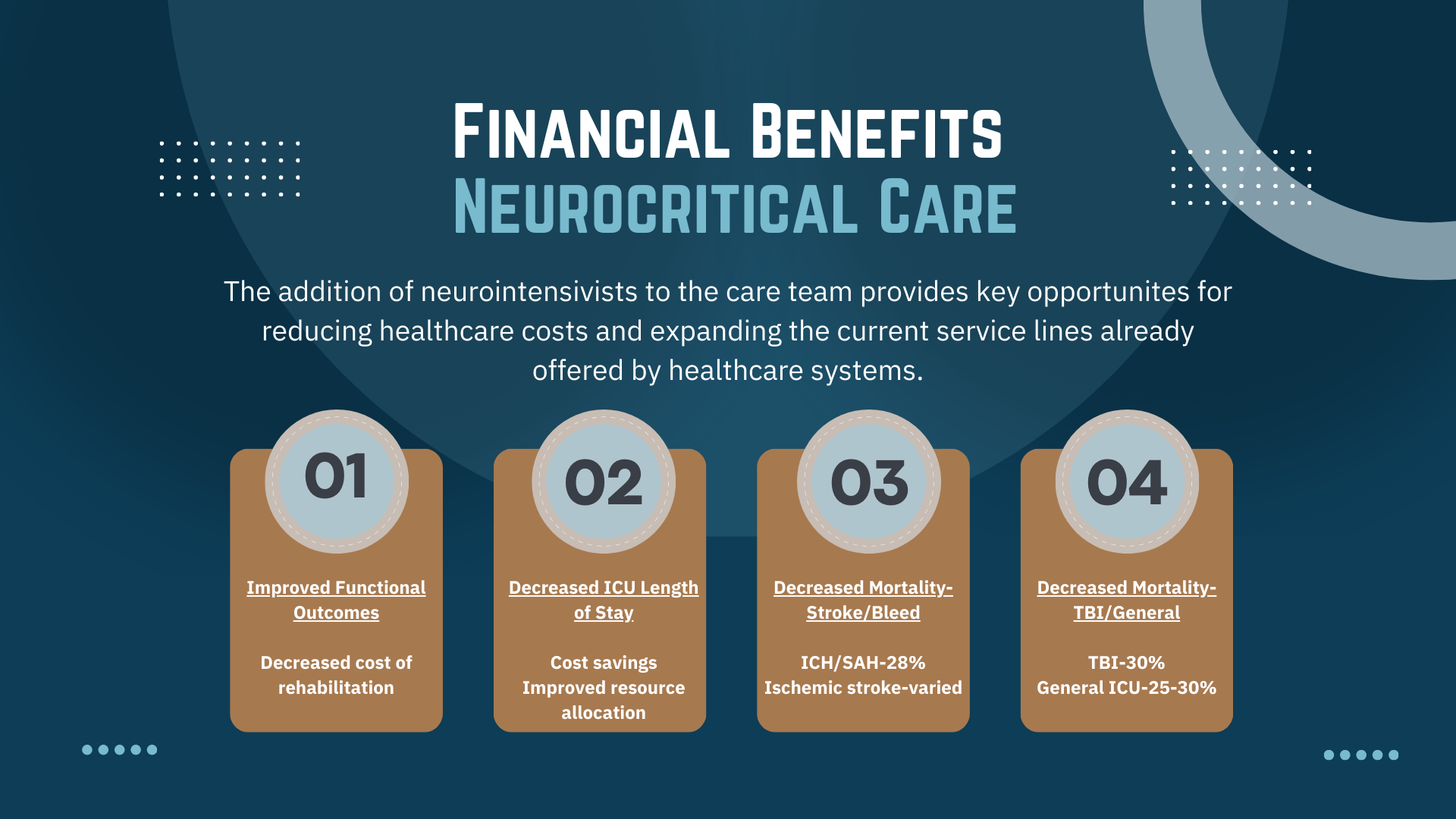
The addition of neurointensivists to the care team provides key opportunites for reducing healthcare costs and expanding the current service lines already offered by healthcare systems.
The addition of neurointensivists to the care team provides key opportunites for reducing healthcare costs and expanding the current service lines already offered by healthcare systems.
The integration of neurohospitalists into the healthcare system enhances revenue opportunities while reducing operational costs.

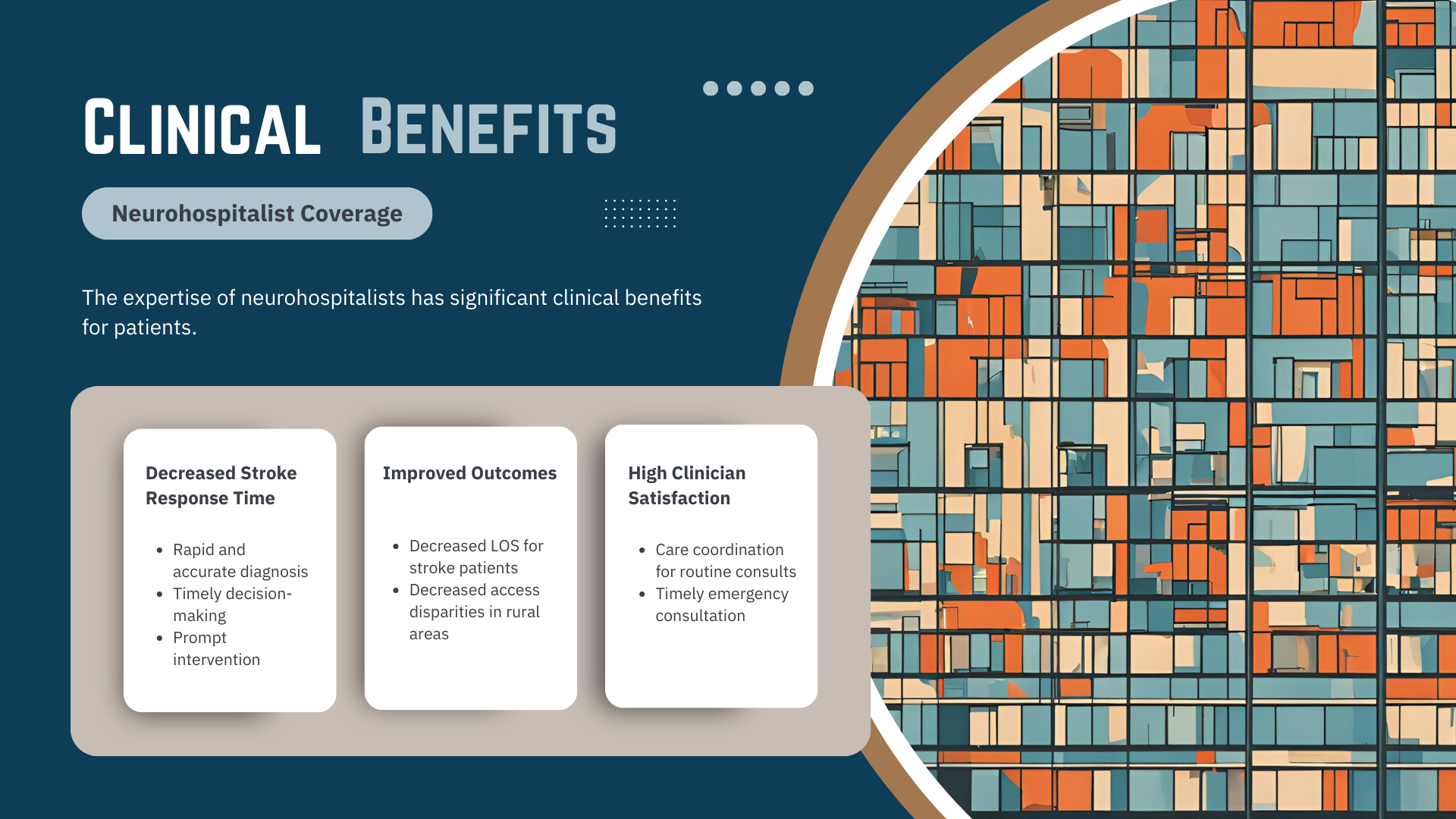
The expertise of neurocritical care providers has significant clinical benefits for patients.

Aggregates data and delivers actionable insights to support informed decision-making, strategic planning, and performance monitoring.
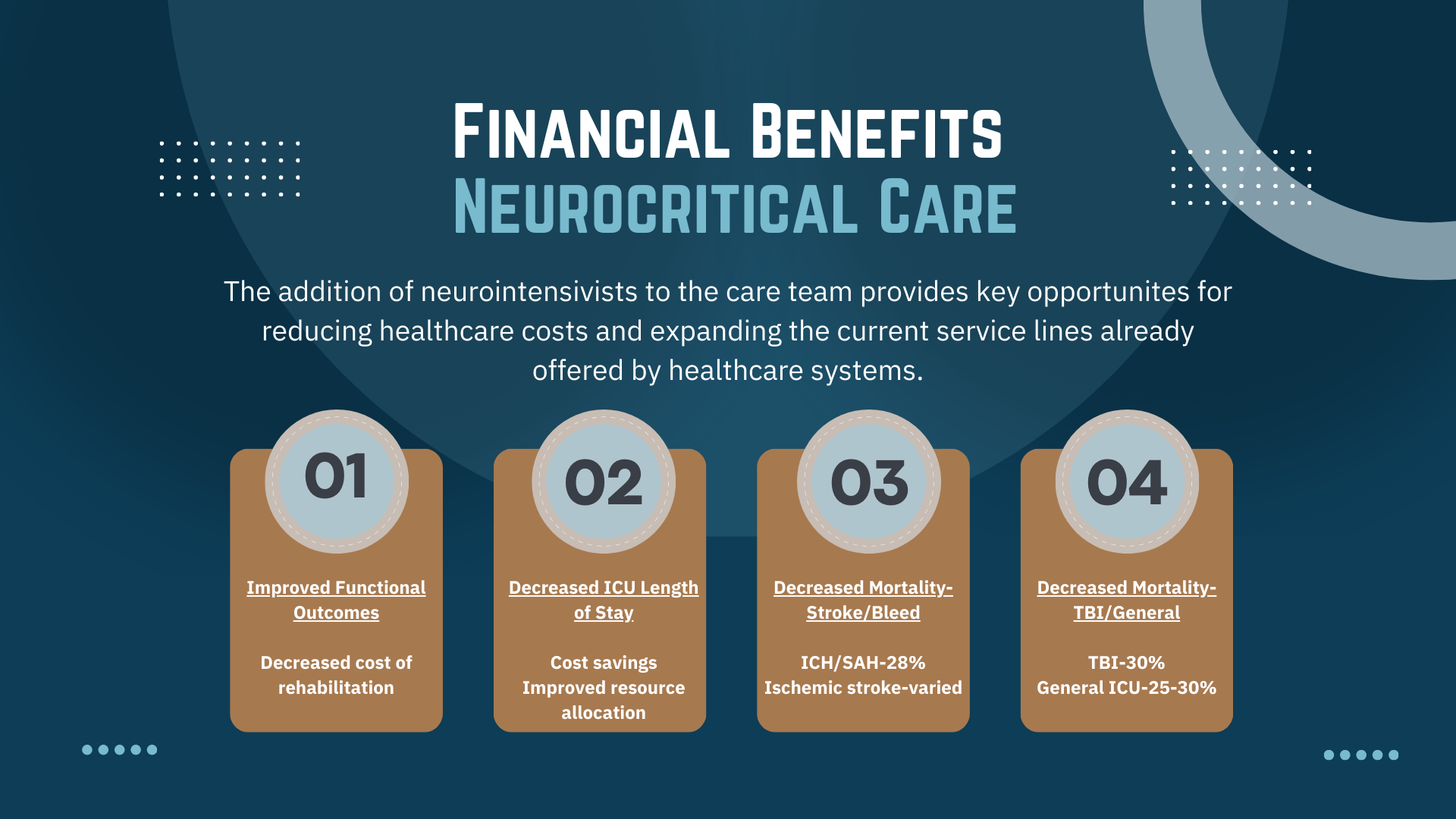
The addition of neurointensivists to the care team provides key opportunites for reducing healthcare costs and expanding the current service lines already offered by healthcare systems.